(Caution – contains graphic images.)
A young Hungarian man with a very good dental chart and healthy tissue had lost a tooth in region 25, which was to be replaced with an implant in his home country. With an Alphatech screw (Alphatech implant) which was aesthetically not located anywhere in the directly visible area of the unprotected tooth-gap, he waited for his prosthetic treatment, until he suffered an accident during the summer vacations.
While kite surfing on Rhodes, another athlete’s cord got caught in the patient’s teeth, exactly in the tooth gap 25. When the other athlete’s parachute was once again steered into the power zone, dental trauma ensued. It was such a strong jolt that teeth 21-24 were torn apart completely from the jawbone. The teeth, together with the buccal bone lamella, drifted to the sea floor. After an on-site basic treatment in Greece, during which the wound was cleaned and the wound edges were approximated, he then came to us for treatment three days later.
In addition to the great trauma suffered by the patient through loss of bone and teeth, it was imperative that it had to be restored as quickly as possible to such a condition, so as to enable him to pursue his career. As the first clarinet of a world-famous orchestra, he was dependent on stable front teeth for lip closure as well as for articulating the sound of the wind instrument. As a professional musician, the patient regularly practiced up to eight hours on the clarinet so as to not lose his technique and approach. Our task, therefore, was to reconstruct not only anatomically and aesthetically, but also to enable playing at this high level during the entire treatment period of six months by means of a stable, resistant form of long-term temporary appliances (Figs 1- 2).

Diagnosis
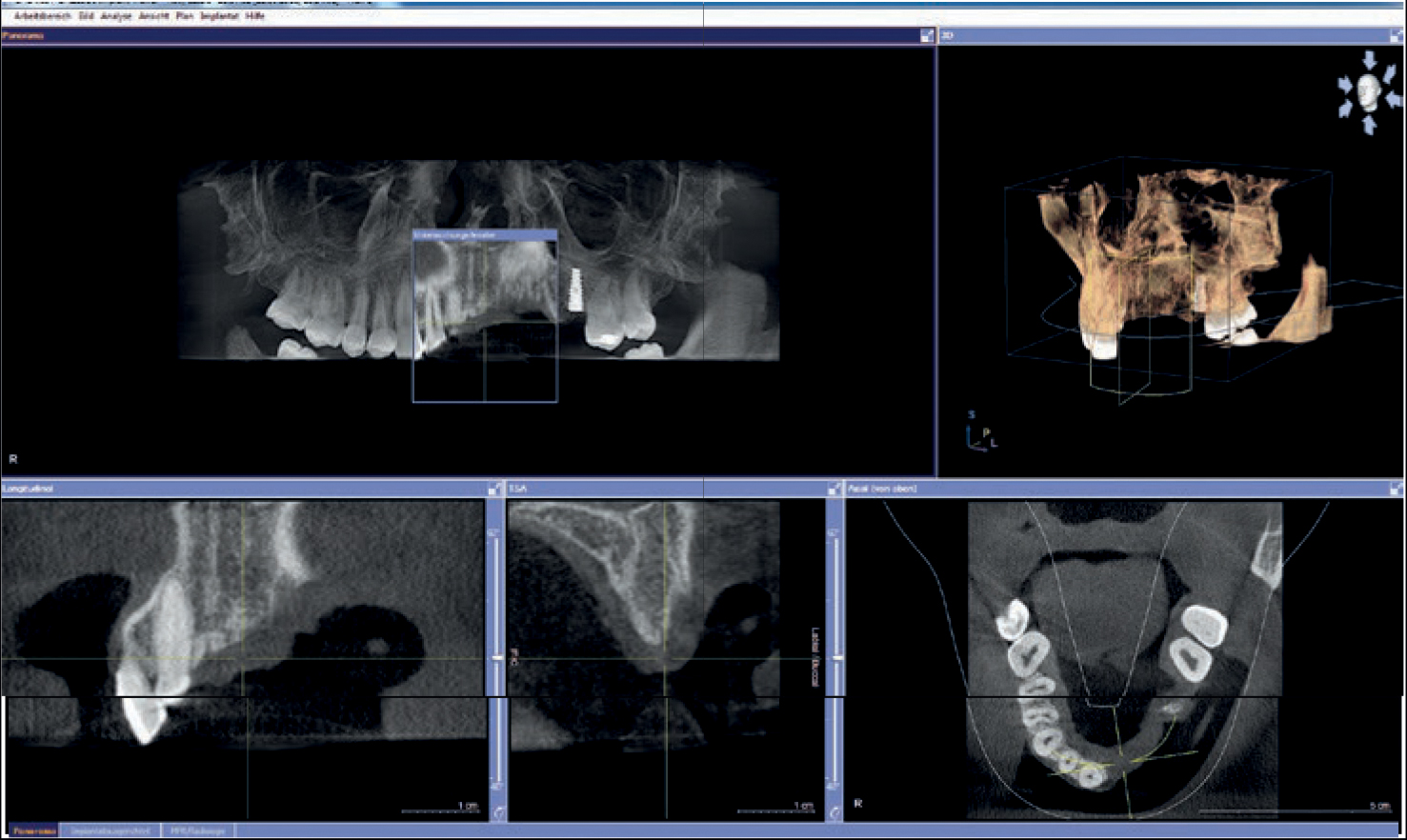
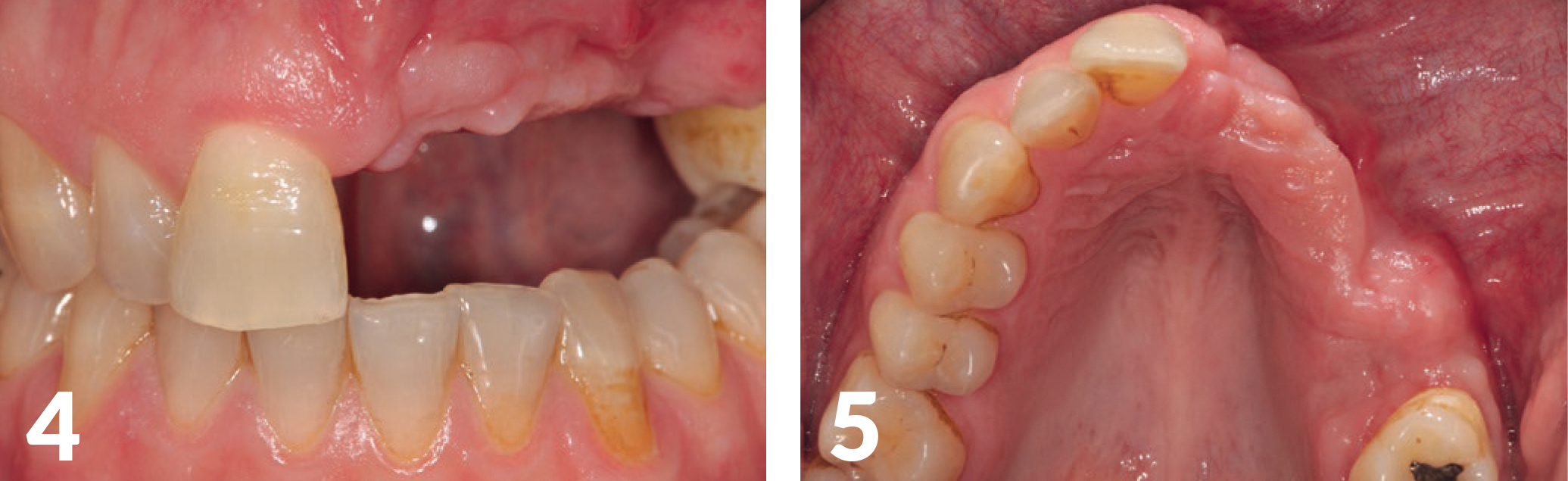
Diagnosis Impression, registration, and photo documentation for the planning of the case, estimation of aesthetics parameters (smile line, lip closure, 3D-defect rewriting); It showed a very extensive defect in the horizontal as well as vertical direction, which confirmed our assumption that this was an extremely demanding case (Figs 3-5).
Planning
Preparation of the treatment strategy and timetable (one-stage, multi-stage procedure, prosthetic treatment options); After defect presentation and evaluation of the soft tissue in combination with the smile-line, planning, clarification, and reconciliation with the patient’s requirements, a long-term temporary appliance in the form of a model cast prosthesis
was manufactured by means of backward planning (Figs 6-7). The patient was able to play the clarinet with this temporary solution without any major restrictions.

Surgical Procedure
Twelve weeks after the accident, we operated for the first and only time.
Our principle is: Compromised tissue does not necessarily get better by increased surgical procedures.
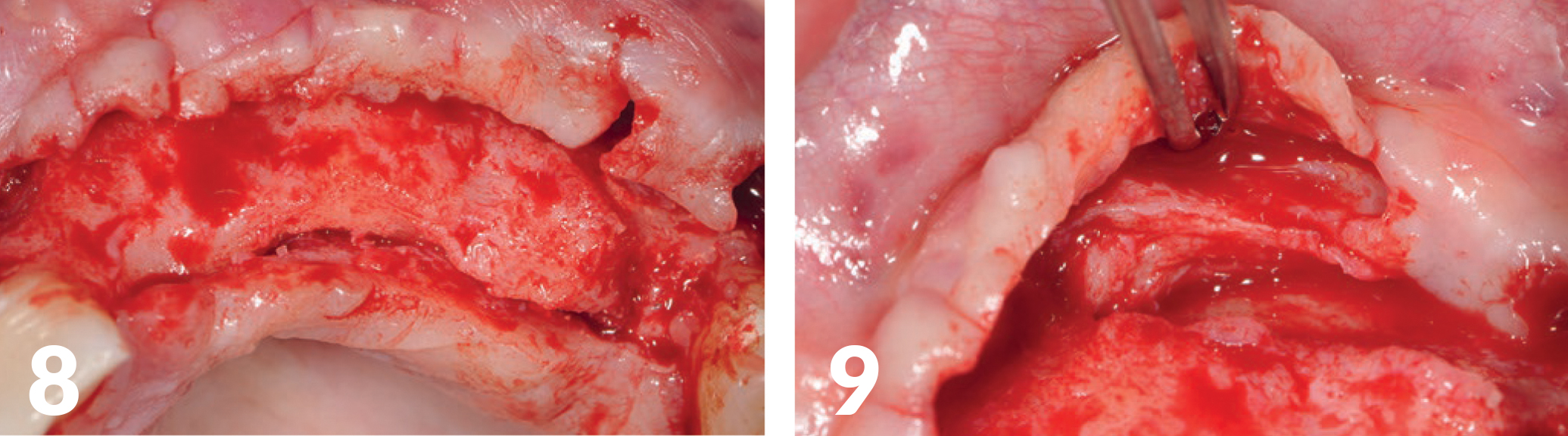
The objective was to create the widest possible basis for dental restorations and to build it as vertically as possible, with a single procedure. Care was taken to ensure the gap was as free of tension as possible, which was urgently required for the amount of augmentation, to ensure good primary wound healing. The incision was from tooth 11 to tooth 26 with vertical relief sections (Figs 8-9).
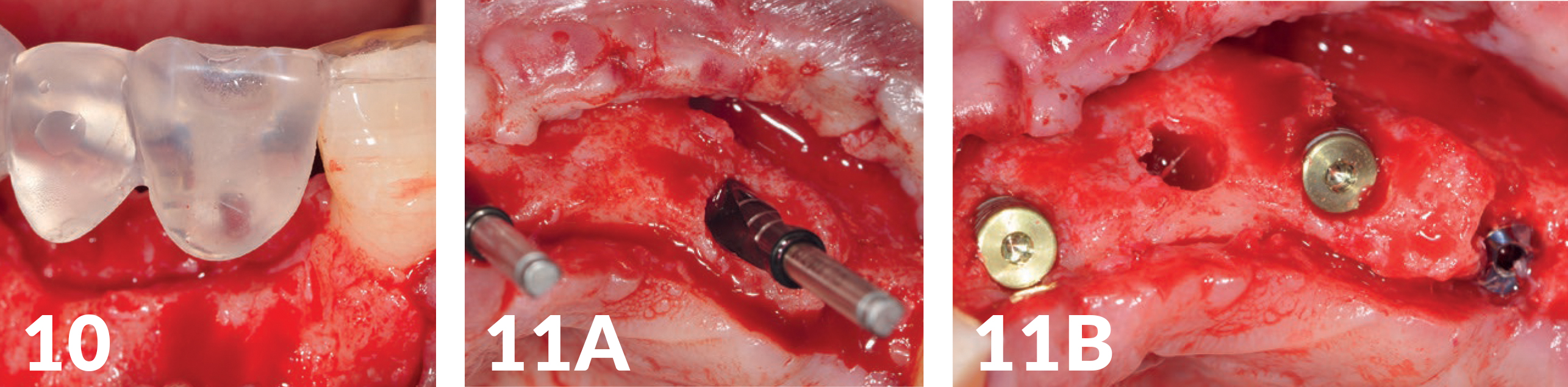
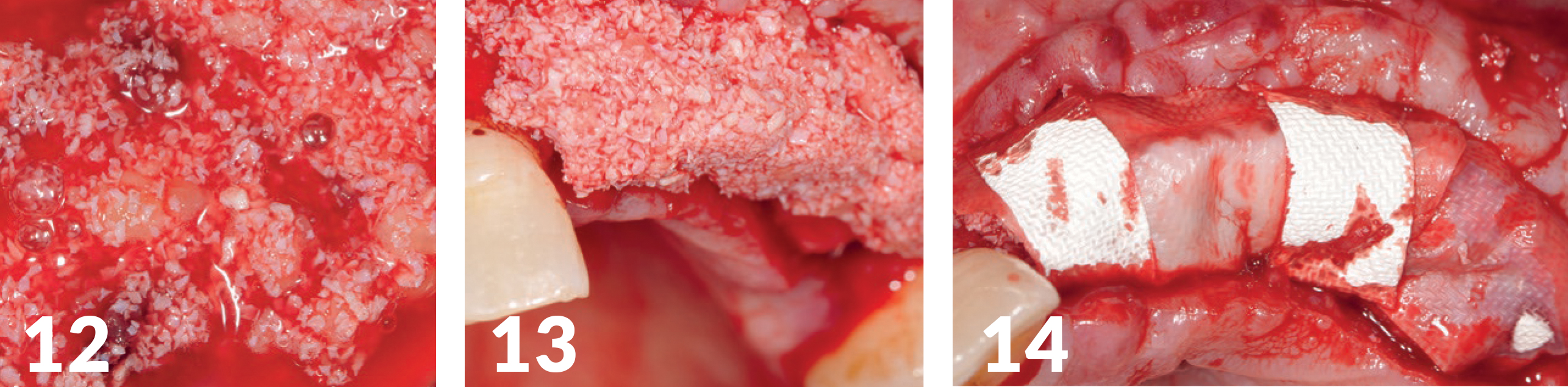
Three NobelActive (Ø 4.3 mm) (manufactured by Nobel Biocare) with a photo-functionalized surface (manufactured by Ushio) were inserted through a drilling template (Figs 10-11B). As augmentation, a mixture of autologous bone was used with THE Graft (distributed by Citagenix), which was also impregnated with i-PRF (Mectron Centrifuge), to produce the so-called sticky bone — a fixed augmentation (Fig 12). The autologous blood of the patient was centrifuged and processed; additionally, we mixed it with PRF (manufactured by Mectron). Covered with several resorbable collagen membranes and a PRF-membrane adapted to the jaw crest, the wound edges could finally be closed without tension (Figs 13-17). The healing period was without complications.
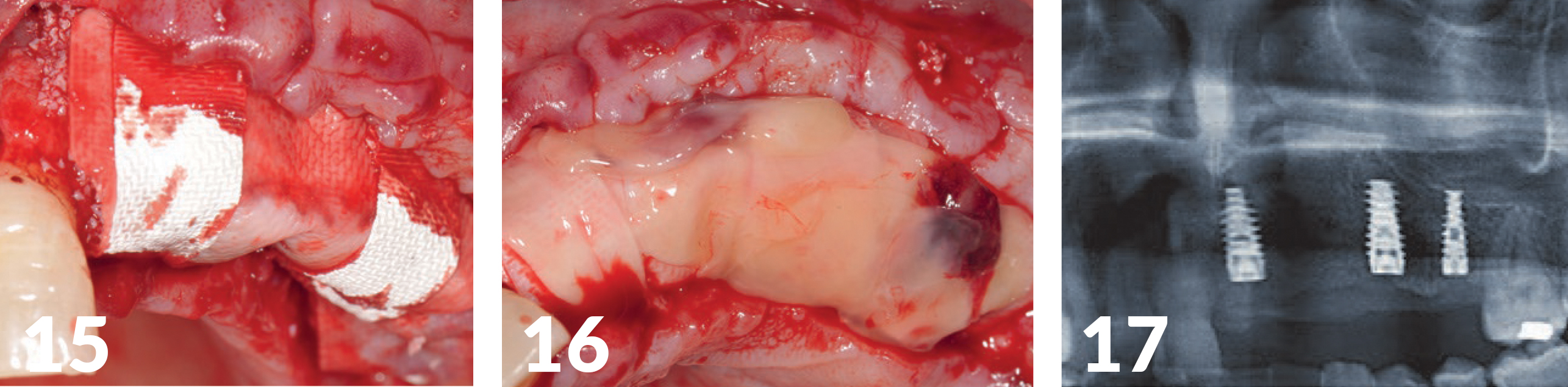
Cut-down/Denudation
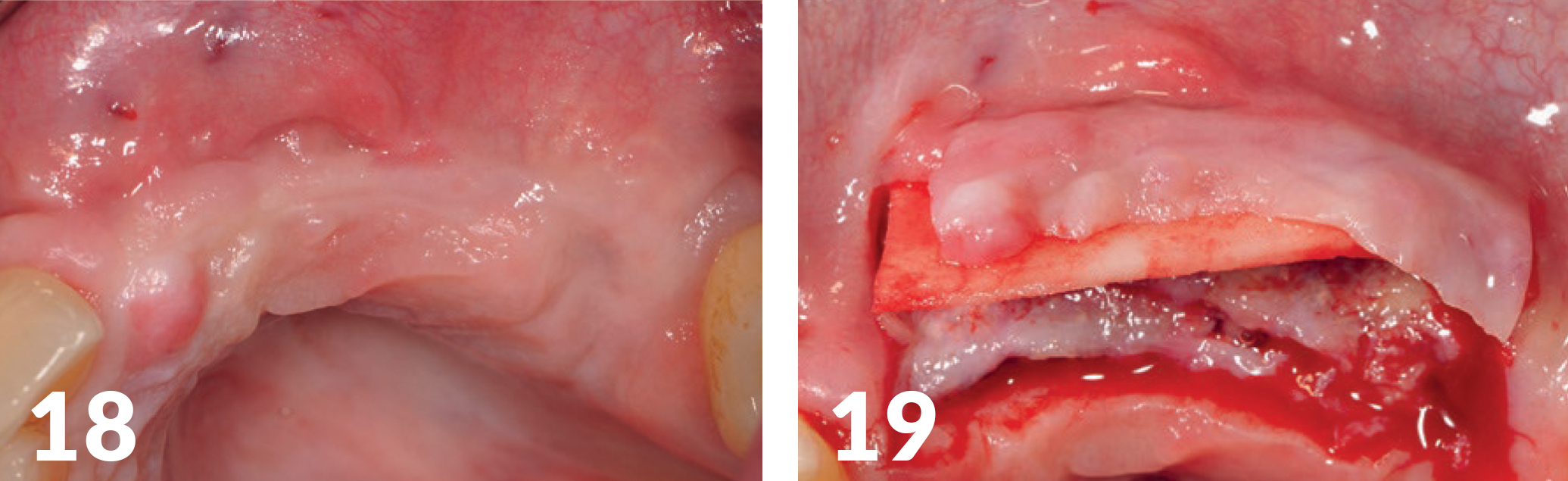
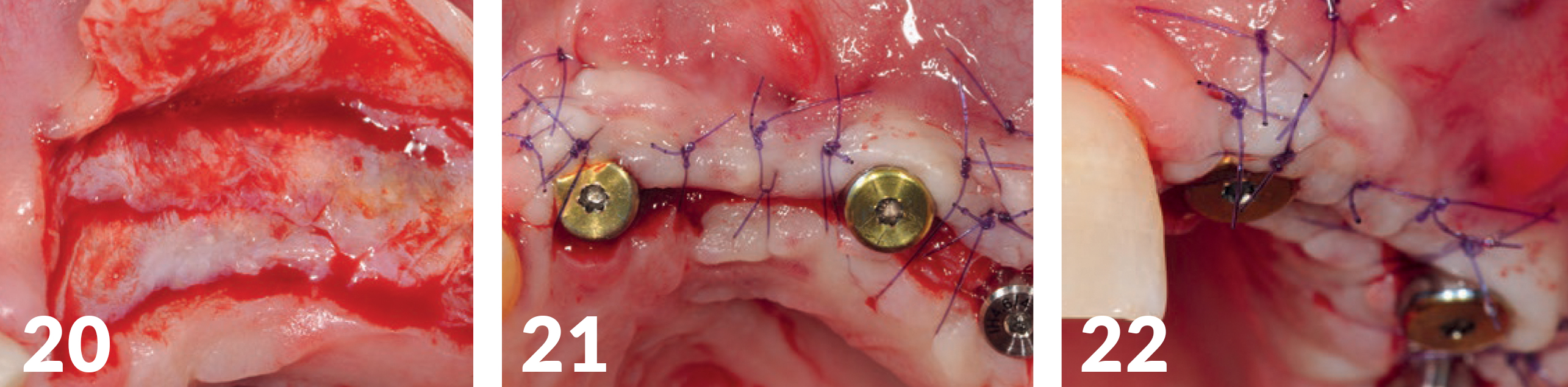
The implants were exposed four months postoperatively, with particular consideration to the former soft tissue architecture and its natural conditions (e.g., sufficient keratinized gingiva around the implants, mucogingival border) (Figs 18-22). In addition, a thickening of the jaw crest was performed via a soft tissue graft (Mucoderm, bot.) (Fig 21), in order to create the conditions for a broad soft-tissue jaw crest base.
Production of the Implant-Supported Bridge Supply Long-Term Temporary Appliance
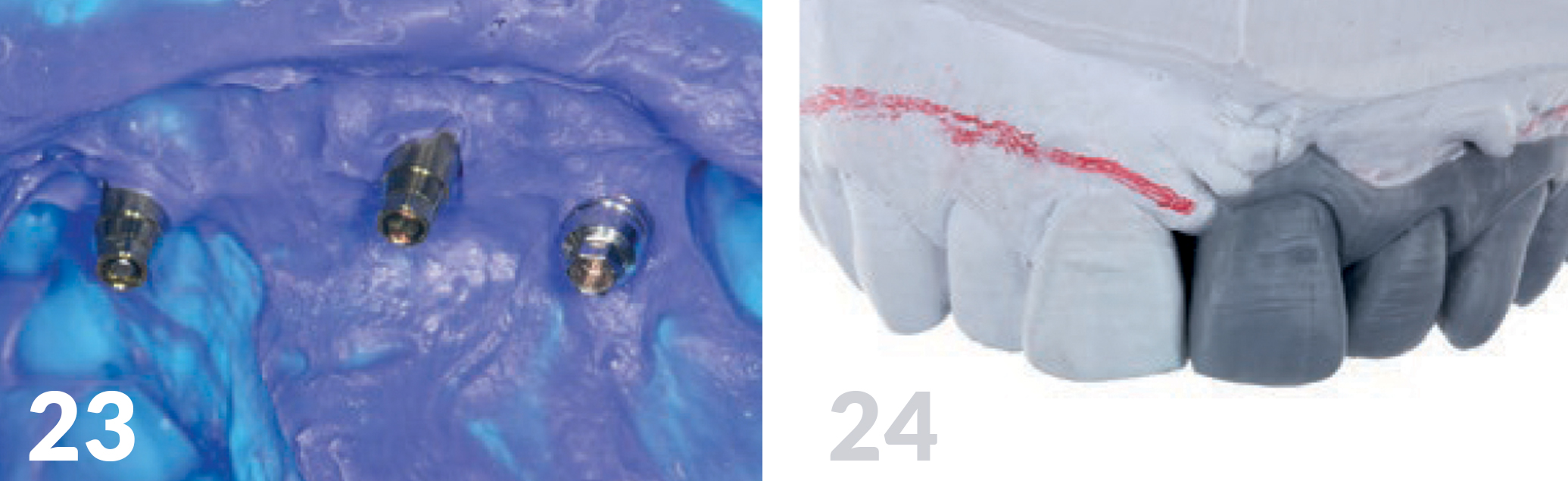
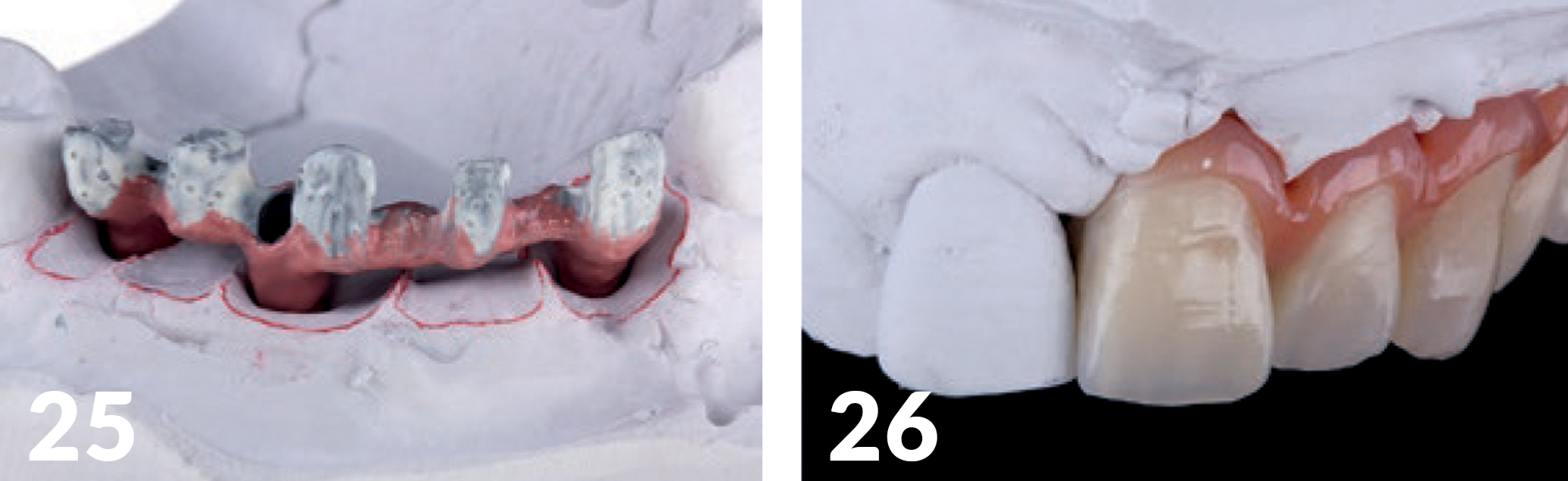
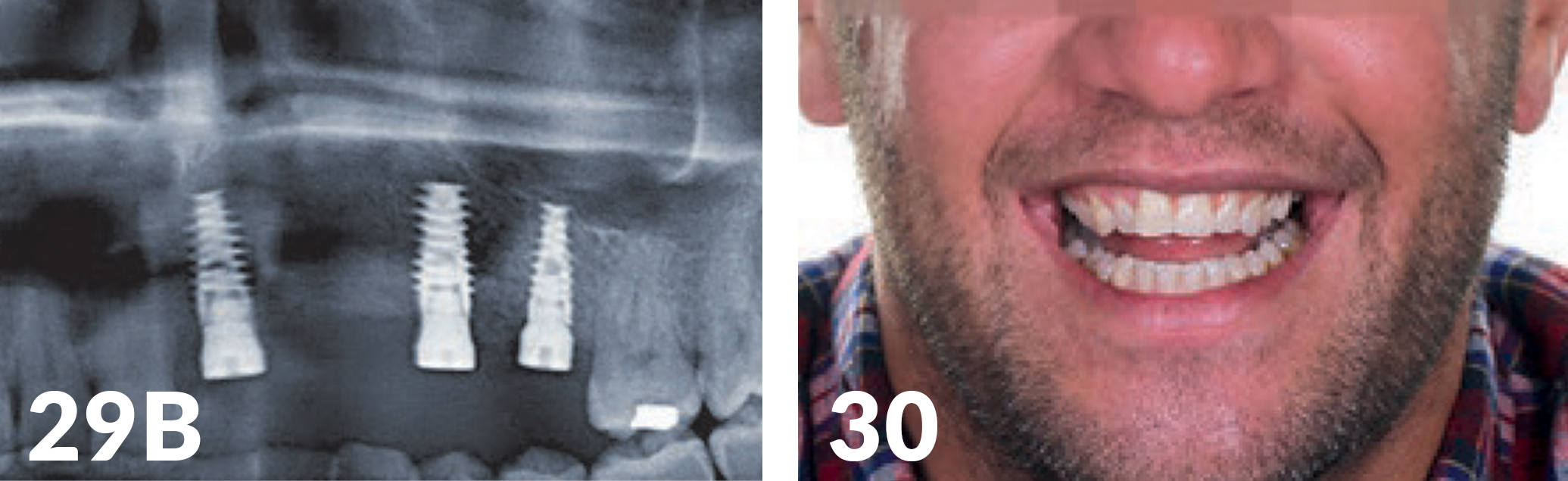
Three weeks after exposure of the implants, an open impression was made for the production of the long-term temporary appliances on the implants (Fig 23). The aesthetic analysis of the models Labside confirmed we had slight deficits in the vertical and had to be compensated for with red aesthetics (Figs 25, 26), but the positioning of the implants was optimal. Just as with the base of the jaw crest, the horizontal plane provided a good basis for achieving an aesthetically appealing shape of the soft tissue using Pontic. (Figs 27 -28). The patient’s smile-line was naturally located in an area (Fig 29a) which did not expose the sulcus transition in the distal region.


Trial and Usage of the Long-Term Temporary Appliances
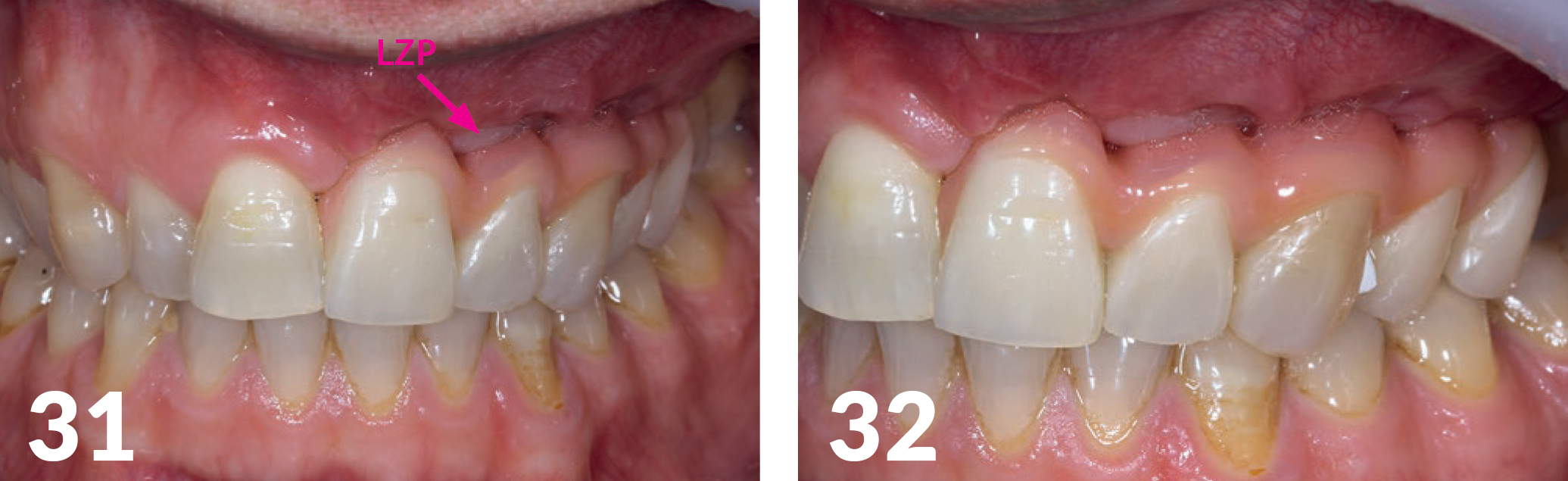
After aesthetics and functional testing, the occlusal bridge was inserted (Fig 30). The patient again had solid teeth, aesthetics, and function, and also, the playing of his instrument was possible without restrictions. The x-ray check (Fig 29b) showed good osseo integration of the implants. During the follow-up, the base of the long-term temporary appliance bridge was under filled and optimally adjusted until the formation of the hard and soft tissue structures remained stable (Figs 31- 32).
Forecast
The prosthetic treatment in the second part of this patient’s case will deal with the further CAD/CAM-assisted implementation of the long-term temporary appliances with ceramic materials. The waiting period of at least four months until the next treatment step was chosen in order to exclude possible soft tissue or hard tissue complications.
 THE Graft™ Syringe by Citagenix |
 THE Graft™ Vial by Citagenix |
|---|

Written by Dr. Peter Randelzhofer, Munich, Germany.
Published in TIPS – July/August, 2022. Submitted by Citagenix.
Category: Merchandise
Back to Articles